In light of a recent string of local cases of COVID-19 in Hong Kong, HKUMed researchers have warned that these cases may indicate a superspreading event is happening in the city.
As previous studies have found that approximately 20% of the cases are responsible for 80% of all transmission events, Professor Gabriel Leung emphasised the importance of contact tracing these 20% of cases in order to effectively control the spread of COVID-19.
However, looking at the daily reported cases alone may not paint the most accurate picture when assessing the severity of an outbreak. As a result, epidemiologists often focus on two key statistics when discussing transmission trends and growth rates – basic reproduction number (R0), and effective reproduction number at time (Rt). Understanding the implications of these two numbers allows governing officials and health systems greater insights into the developmental trends of the outbreak, and therefore a more accurate assessment of effectiveness in public health protocols, allocation of bed spaces at hospitals etc.
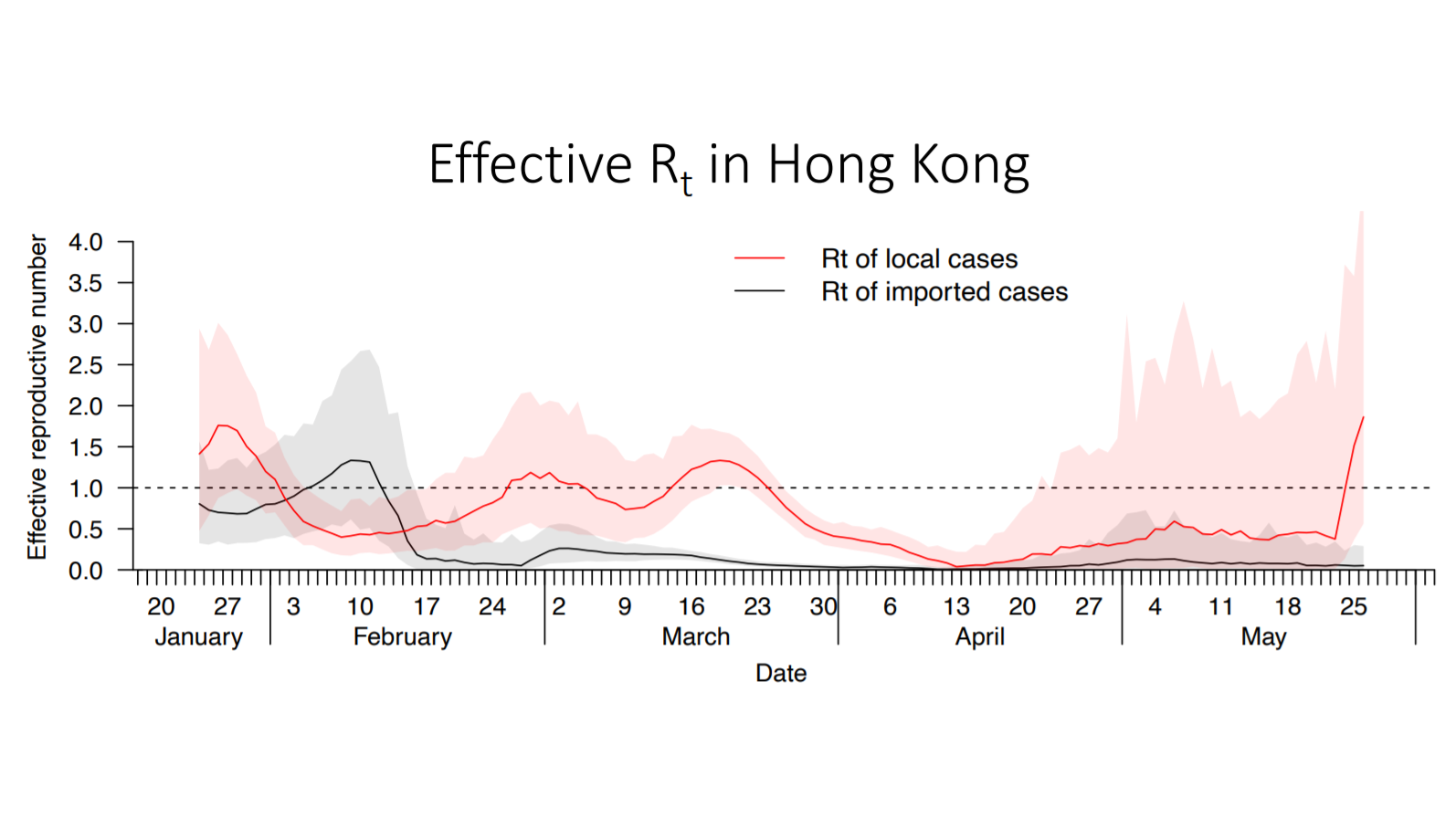
As of 26 May, the effective reproduction number (Rt) of COVID-19 in Hong Kong is approaching 2, signalling the possibility of further outbreaks. This is a reminder that we should be flexible with preventive measures in order to best control the disease,
A real-time dashboard published by the School of Public Health at HKUMed is now accessible for all, making it easier to follow daily infection numbers, and updated effective reproduction number at time: https://covid19.sph.hku.hk/dashboard
We have also invited members of the research team at the School of Public Health to explain the significance of these published statistics and how we can interpret them in order to best understand the progression of the current coronavirus outbreak.
Q1. What is the ‘basic reproduction number’ (R0) and ‘effective reproduction number at time’ (Rt)?
Basic reproduction number (R0)
- Pronounced as “R-naught”; R0 reflects the number of people that one infected person can potentially go on to infect if there are no intervention measures in place.
- This number is inherent to each pathogen, but it may vary depending on environmental factors such as population density and contact patterns.
- The new coronavirus has an R0 of 2.2, which means that each infected patient of the virus may go on to further infect around two more people should there be no intervention protocols in place.
- Rt is the average number of secondary cases per one case at any given time. This number will vary as the outbreak progresses, and indicates real-time transmissibility.
- Effective control measures and behavioral changes, such as quarantine enforcement, usage of face masks, travel restrictions, class suspensions, and social distancing, are all factors that may affect the Rt of a virus.
Rt > 1
Each infected patient will go on to infect on average more than one person. Should secondary infections occur (i.e. new clusters of infection), the number of infected cases will increase exponentially, further exacerbating the pandemic over time.
Rt = 1Each infected patient will go on to infect one other person. Statistically, this would mean that one new infected patient will replace another who had recovered or passed away from the disease. This also suggests that the outbreak is stabilising, with no changes in number of infected people over time.
Rt < 1Each infected patient will go on to infect on average less than one person. If this number is maintained over the course of two to three weeks, it means that fewer people are being infected which suggests the outbreak is slowing down over time.
Q3. Assuming Rt goes below 1, is the outbreak over?
While it may be encouraging to see Rt go below 1, this does not necessarily mean we can immediately relax current health protocols and precautions, as there are other factors to consider as well, such as the number of confirmed cases, demographic composition, and availability of medical resources.
For example, if a double-digit daily growth of confirmed cases is observed in a population of ten million, then Rt of 1 would be acceptable. However, should the daily growth reach triple or even quadruple digits, then the same Rt rate of 1 would pose additional implications in terms of outbreak potential. All in all, it is crucial for communities to remain vigilant in order to suppress the Rt number as much as possible (i.e. maintaining it at 0.1 to 0.2) for a sustained amount of time, as only then would the outbreak be possibly contained.
Since January, HKUMed researchers have been conducting interviews on citizens’ attitudes towards preventive measures against COVID-19. While over 90% of the respondents say they have been wearing masks, the use of a mask is “necessary but insufficient” on itself in preventing COVID-19 transmission, according to the team.
Other measures, such as work-from-home arrangements and social distancing, should also be practised.
The team recommends that Hong Kong improve its COVID-19 testing capacity (especially for high-risk groups) in both public and private health care, and also scale up contact tracing capacity.