Numerous countries around the world are now seeing local outbreaks of COVID-19, and in some cases within communities as well. Following the latest estimated fatality rate of 1.4% as announced by HKUMed WHO Collaborating Centre for Infectious Disease Epidemiology and Control today at a press conference, many are curious to know how this statistic was obtained, and reasons for its discrepancy with previously published statistics from other outlets.
In view of these questions, our research team from the School of Public Health has provided some clarifications.
Q1. How is fatality rate calculated? Are there different ways of calculation that may result in discrepancies?
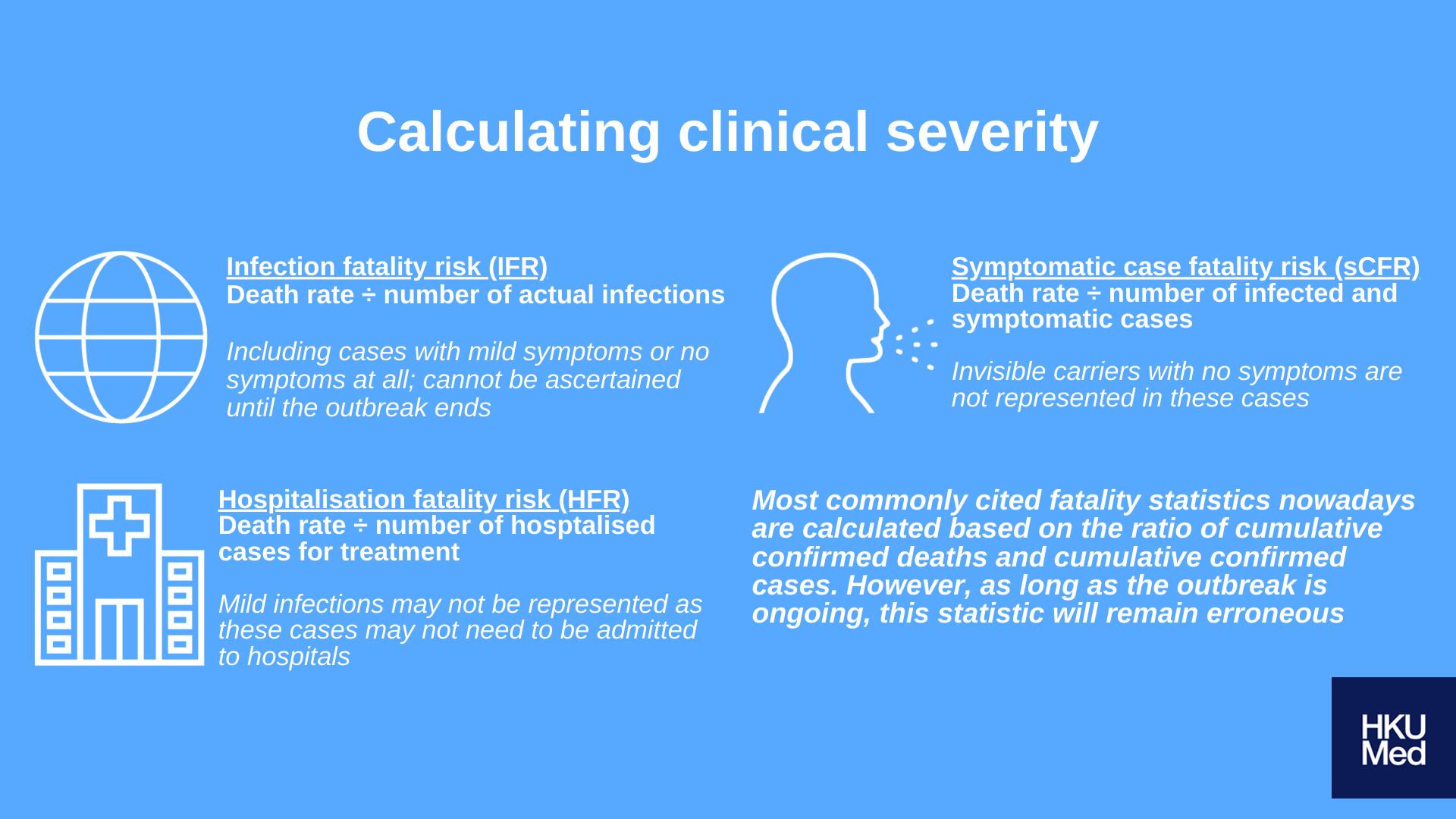
We must first consider three distinct definitions of fatality risk:
- Infection fatality risk (IFR): Death rate ÷ number of actual infections
- Symptomatic case fatality risk (sCFR): Death rate ÷ number of infected and symptomatic cases
- Hospitalisation fatality risk (HFR): Death rate ÷ number of hosptalised cases for treatment
These three definitions differ in the denominational factors i.e. number of actual infections, infected and symptomatic cases, and hospitalized cases respectively. Such differences may result in discrepancies between calculations and actual real-life contexts.
Most commonly cited fatality statistics nowadays are calculated based on the ratio of cumulative confirmed deaths and cumulative confirmed cases. However, as long as the outbreak is ongoing, this statistic will remain erroneous: in most cases, the progression of infection can typically be ascertained only after two to four weeks; the calculation is hence not reflective of the progression of infection. In addition, some countries may not have sufficient testing kits to conduct widespread testing, resulting in many unidentified cases that are excluded from the census.
As for calculations of HFR, it is focused on hospitalised cases, but fails to take into account mild cases of infection where medical attention in hospitals may not be required; this is especially true for any asymptomatic cases.
In view of the above limitations, the current calculated fatality risk of 1.4% is based on calculating the sCFR, as it is comparably more accurate than IFR or HFR in our current context. There are of course limitations to this method of calculation too, as it does not take into account asymptomatic cases.
Q2. A fatality rate of 1.4% seems very low. Does that mean we may resume our regular daily routines?
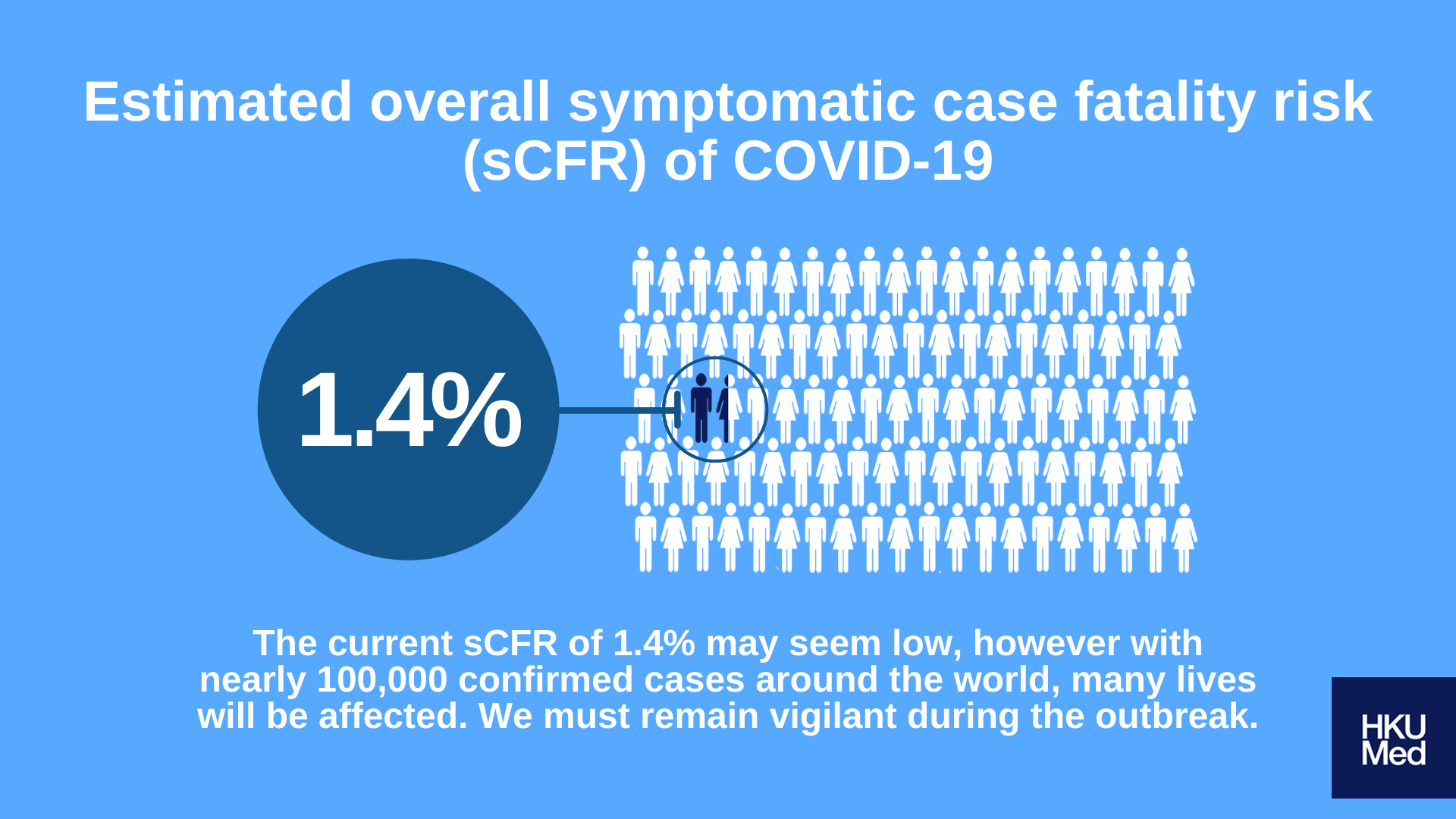
In comparison to outbreaks of similar scale in the past, it is indeed accurate to say the current COVID-19 outbreak is less severe compared to the 1918 influenza pandemic for example. That being said, this current outbreak poses greater threats compared to the 2009 flu pandemic, which means that all prevention measures must remain enforced.
Current statistics are calculated based on the number of confirmed cases with symptoms; despite the seemingly low fatality rate of 1.4%, current number of confirmed cases are nearing 100,000 globally, with possibly many more asymptomatic cases. Countless lives will be affected because of this outbreak, and as such requires a high level of caution still.
We understand that many are frustrated at the seemingly endless outbreak, with additional stressors stemming from suspended social functions and recreational activities. However, social distancing remains the most effective way in protecting oneself and their loved ones, and should be strictly enforced throughout the outbreak despite its many difficulties.
Q3. Is age a factor that affects likelihood of infection?
Research studies suggest that those above the age of 70 are three times more likely to be infected, as well as three times more likely to suffer fatal complications compared to those below the age of 70. Taken altogether, the overall severity of impact on the older population is nine times that of the average population.
As a community, additional care and support must be given to the elderly; this can be achieved by ensuring sufficient supply of healthcare resources to them. We must also enforce health precautions on their behalf, and spare no efforts in minimising possibilities of an outbreak in elderly homes or other spaces where elderly populations are likely to gather.
For more information on the research, click here.